A review of the evolution of surgical treatment, systemic chronicity, and the role of artificial intelligence in precision medicine.
By Ehab Soltan
HoyLunes — Congenital heart disease (CHD) represents the most frequent structural malformation, with a global prevalence stabilized between “8 and 10 cases per 1,000 live births.” However, the most disruptive data point is not its incidence, but its current demography: in developed countries, survival exceeds “90%”.
This success has generated a new clinical population: “ACHD” (Adults with Congenital Heart Disease). It is estimated that in the US alone, more than “1.5 million adults” reside with CHD, surpassing the number of pediatric patients for the first time in history. According to the “ESC/AHA” guidelines, this shift forces a displacement of focus from anatomical correction toward the management of late morbidity.

Surgical Evolution: From Rescue to Functional Anatomy
It is imperative to avoid anachronisms. While the “Mustard and Senning” techniques were milestones in the transposition of the great arteries (TGA), today they are considered procedures of historical or rescue value. The contemporary gold standard is the “arterial switch (Jatene procedure),” which restores anatomical ventriculo-arterial concordance, minimizing the risk of systemic right ventricular failure in the long term.
Nevertheless, chronicity persists in complex palliations such as the “Fontan circulation”. The pathophysiology of the Fontan —a passive circulation without a pulmonary ventricular pump— entails inevitable systemic complications:
Fontan-associated liver disease (FALD).
Protein-losing enteropathy.
Atrial arrhythmias due to scar remodeling.
Structural Interventionism: The Era of Hybrid Procedures
Although medical rhetoric suggests the “end of the sternotomy”, the clinical reality is more nuanced. As noted by “Kenny et al. (JACC Cardiovascular Interventions)”, the trend is not substitution, but rather “hybrid integration.” Open-heart surgery remains the pillar for complex reoperations, Fontan failures, and heart transplants. Innovation lies in the use of catheterization for the “implantation of transcatheter pulmonary valves (TPVI)” and the closure of residual defects, reducing the cumulative burden of interventions that the patient must face throughout their life.
The Biology of the “Repaired Heart”
The concept of the “repaired heart” is a simplification of a complex biological phenotype. Surgery restores hemodynamics but does not reverse an “altered embryological development”. From the prenatal stage, deviated molecular signaling conditions a myocardium with a distinct cellular architecture, characterized by the disorganization of myocytes and an extracellular matrix predisposed to “interstitial fibrosis”.
This substrate, combined with “chronic ventricular remodeling,” establishes the basis for late systolic dysfunction. At a systemic level, these patients manifest “persistent endothelial dysfunction”. Exposure to non-pulsatile flows alters vascular autoregulation, impacting the “neurovascular axis”. This explains the vulnerability to subclinical ischemic events and the high prevalence of anxiety, depression, and executive deficits documented in contemporary literature.
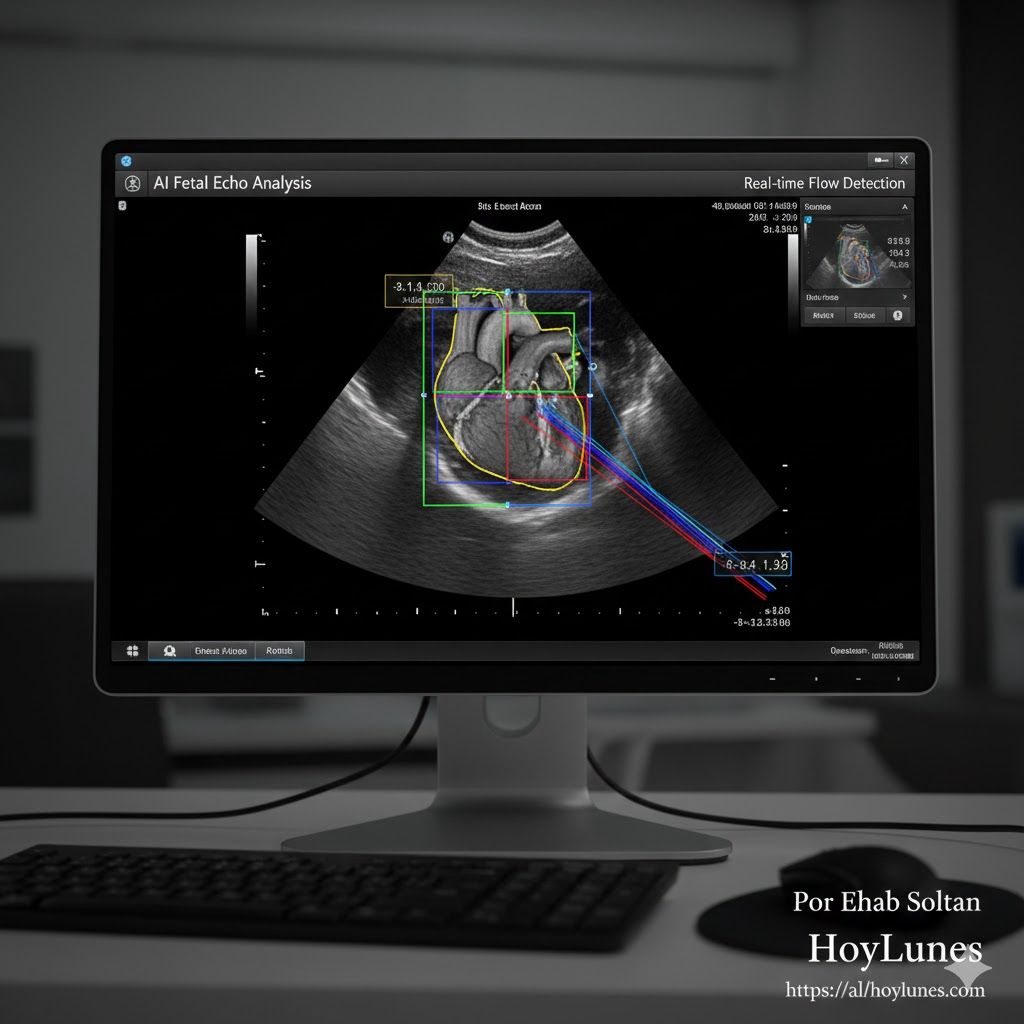
Artificial Intelligence: Fetal Diagnosis and Flow Analysis
AI in fetal cardiology has moved from hypothesis to validation. The work of “Arnaout et al. (Nature Medicine, 2021)” demonstrated that deep learning models can equal experts in identifying critical echocardiographic views. Today, its real utility is summarized in the “reduction of diagnostic omissions” and in “predictive analysis”. Following “Diller et al. (EHJ, 2021)”, AI allows for the processing of massive volumes of cardiac MRI data to identify biomarkers of heart failure before they become clinically evident.
Programmed Multi-Organ Failure: The Fontan Challenge
The Fontan case represents the paradigm of “central venous insufficiency.” By chronically elevating venous pressure, retrograde congestion is triggered with consequences for hepatic microcirculation. “Fontan-Associated Liver Disease (FALD)” necessitates the integration of elastography protocols and hepatobiliary monitoring. Understanding CHD as a multi-organ pathology is the only way to guarantee functional longevity.
The cardiology of congenital heart disease has completed its first major transition: from success in the operating room to the management of chro
nicity. However, the challenge of the 21st century is to delve deeper into precision medicine, where genomics and artificial intelligence allow us to anticipate systemic organ failure. It is not enough to repair the heart; we must manage the biological trajectory of an organism that survives under unique hemodynamic laws.

Clinical Pearls for Current Practice (Take-home messages)
ACHD Transition: Coordination between pediatrics and adult cardiology is the critical link for 90% of survivors.
Advanced Imaging: Cardiac MRI is the standard for evaluating fibrosis and ventricular volumes in the repaired heart.
AI as a Filter: Reduces inter-observer variability and diagnostic omission in lower-volume centers.
Sources and Bibliographic References
Arnaout, R., et al. (2021). ´Nature Medicine´. “Deep learning-assisted fetal echocardiography”. [https://www.nature.com/articles/s41591-021-01362-7]
Diller, G. P., et al. (2021). ´European Heart Journal´. “Artificial Intelligence in Adult Congenital Heart Disease”. [https://academic.oup.com/eurheartj]
Kenny, D., et al. (2024). ´JACC Cardiovascular Interventions´. “Transcatheter Interventions in Congenital Heart Disease”. [https://www.jacc.org/journal/jcin]
Kovacs, A. H., et al. (2009). ´Circulation´. “Psychological outcomes and neurocognitive deficits in ACHD”. [https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.108.840389]
Topol, E. (2019). ´Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again´. Basic Books.
#CongenitalCardiology #ACHD #PrecisionMedicine #CardiacPathophysiology #AIinHealth #HeartFailure #FontanPhysiology #HoyLunes #EhabSoltan