Pathophysiological implications, advanced neuroimaging biomarkers, and secondary prevention strategies in the preservation of functional autonomy.
By Ehab Soltan
HoyLunes – Contemporary cerebrovascular disease demands a transition from an episodic care model toward one of structural chronic disease management. A critical proportion of ischemic events originates from the occlusion of deep penetrating arteries, resulting in small-dimension infarcts—generally <15 mm—termed «lacunar strokes».
Despite their sometimes subtle clinical presentation, these events constitute the phenomenological expression of «Cerebral Small Vessel Disease» (CSVD). This systemic pathology represents between 20% and 25% of global ischemic strokes and is the primary determinant of vascular dementia and mixed cognitive impairment.
Pathophysiology: The concept of «silent infarct burden»
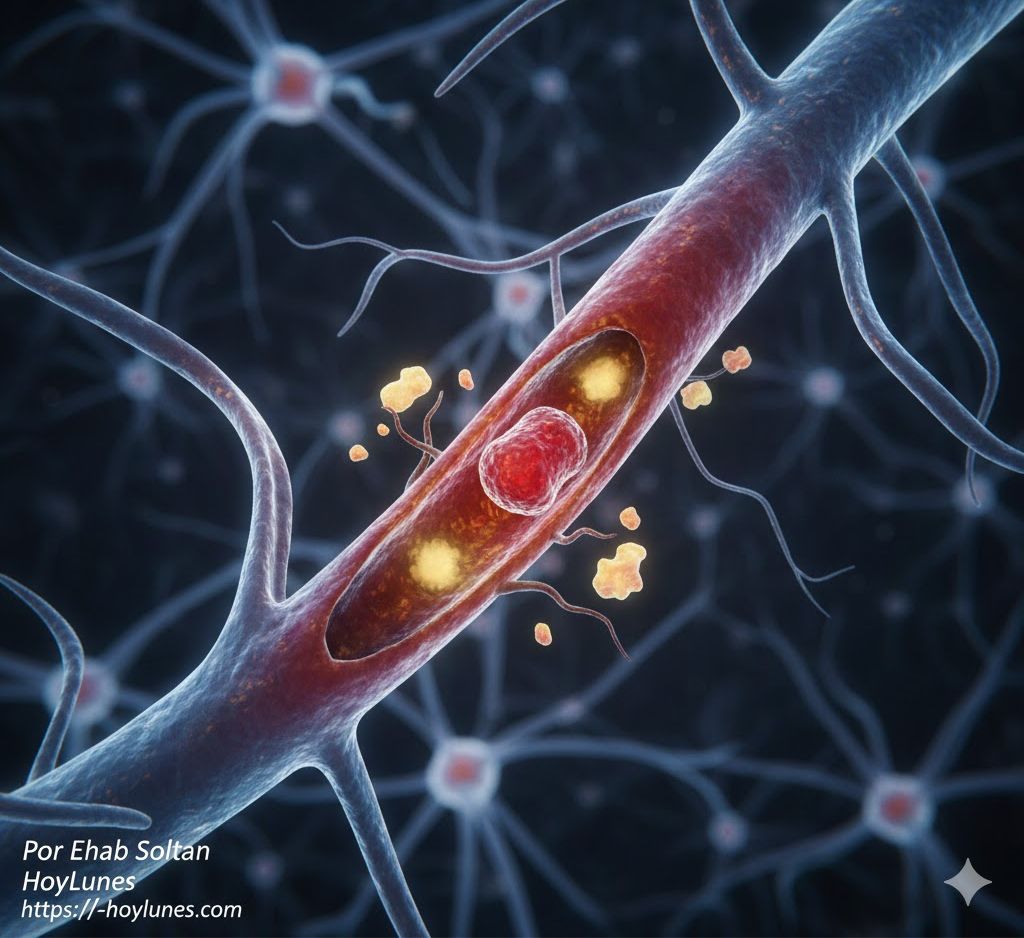
CSVD is not a sudden event, but rather a cumulative process driven by lipohyalinosis, arteriolosclerosis, and chronic endothelial dysfunction. The damage is focused on strategic subcortical regions: basal ganglia, thalamus, internal capsule, and pons.
Current scientific literature emphasizes that the acute manifestation is only the «tip of the iceberg». The «silent infarct burden» refers to lesions detectable through neuroimaging that did not produce an evident focal neurological deficit, but which erode the patient’s cognitive reserve.
Advanced Neuroimaging: Structural Correlates
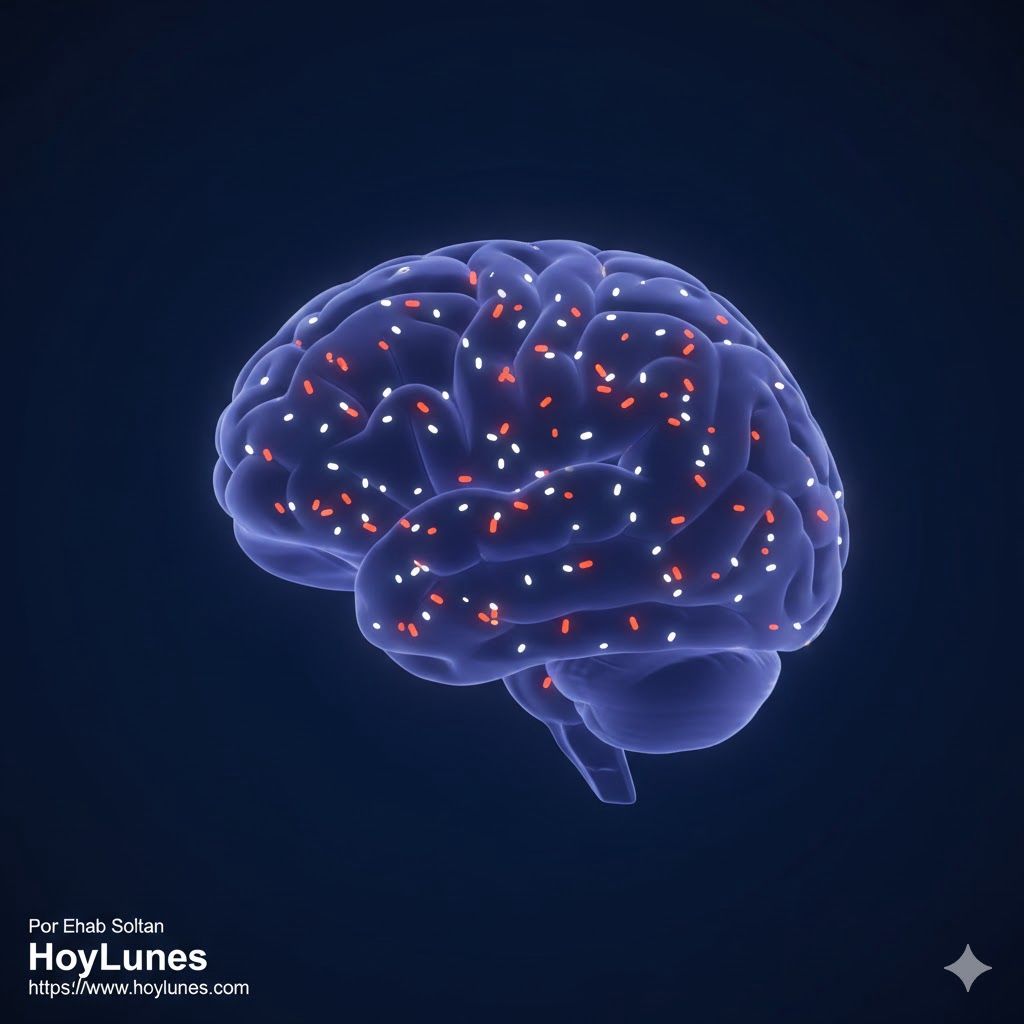
Precision diagnosis and risk stratification depend on Magnetic Resonance Imaging (MRI) protocols that include specific sequences to identify the disease ‘burden’:
FLAIR (Fluid-Attenuated Inversion Recovery) Sequences: Essential for identifying «white matter hyperintensity» (leukoaraiosis), which reflects vasogenic edema, demyelination, and axonal loss.
SWI (Susceptibility Weighted Imaging) Sequences: Allow for the detection of «cerebral microbleeds», critical markers of capillary fragility and hemorrhagic risk.
T1/T2 Sequences: For the characterization of chronic lacunar infarcts and the dilation of perivascular spaces.
The integration of these findings allows for the calculation of a total CSVD burden score, which correlates directly with long-term functional prognosis.
The challenge of differential diagnosis: Aging or pathology?
The most transcendent clinical expression of recurrent lacunar infarcts is often insidious and is frequently mistakenly confused with physiological aging. The alteration of fronto-subcortical circuits leads to:
Executive dysfunction: Difficulty in planning and decision-making.
Psychomotor slowing: Reduction in information processing speed.
Gait alterations: Short steps and a wide base, with an increased risk of falls.
Vascular depression: Affective changes originating from the disconnection of deep neuronal networks.
Advanced prevention and biomarkers: The lesson of SPRINT-MIND
Arterial hypertension (HTN) is the most potent modifiable risk factor. However, evidence suggests that the therapeutic objective must be more ambitious than stipulated in previous decades.
The «SPRINT-MIND» trial demonstrated that intensive systolic blood pressure control (target <120 mmHg) significantly reduces the risk of mild cognitive impairment and the progression of white matter lesions compared to standard treatment (<140 mmHg).
The secondary prevention strategy must be multimodal:
Intensive blood pressure control: Special attention to ‘non-dippers’ (those who do not present the physiological drop in pressure during sleep).
Metabolic management: Strict control of glycated hemoglobin (HbA1c) and lipid profile.
Antiplatelet Therapy: Adapted to the risk profile of ischemia versus hemorrhage (especially in the presence of microbleeds on SWI).
Indirect Neuroprotection: Regular aerobic exercise has been shown to improve cerebral blood flow and synaptic plasticity, acting as a flow modulator in the small vessel.

For reference hospital practice, the approach to lacunar stroke must be structured under the following pillars:
Prevalence: Represents «20-25% of ischemic strokes» worldwide.
Nature: It is a systemic manifestation of «cerebral small vessel disease».
Cognitive Risk: Its recurrence and the cumulative burden are robust predictors of «vascular cognitive impairment».
Critical Factor: «Poorly controlled hypertension» (especially nocturnal) is the main modifiable risk factor.
Diagnostic Standard: «Early and advanced neuroimaging» (FLAIR/SWI) is mandatory to differentiate stroke from aging changes and to establish secondary prevention strategies.
The preservation of cognitive autonomy in the aging population depends on the institutional capacity to detect and treat silent vascular damage before the lesional load becomes irreversible.
References
Fisher CM. Lacunar strokes and infarcts. ´Stroke´. 1991.
Wardlaw JM et al. Neuroimaging standards for research into small vessel disease. ´Lancet Neurology´. 2013.
American Heart Association. Small Vessel Disease and Stroke. AHA Journals.
National Institute of Neurological Disorders and Stroke (NINDS). Stroke Information Resources.
European Society of Hypertension. 2018 ESC/ESH Guidelines for the management of arterial hypertension.
Williamson JD et al. Effect of Intensive Blood Pressure Control on Probable Dementia (SPRINT-MIND). ´New England Journal of Medicine´. 2019.
#LacunarStroke #Neuroscience #BrainHealth #CognitiveImpairment #SmallVesselDisease #Neuroimaging #StrokePrevention #EhabSoltan #HoyLunes