From the “war against the pathogen” to the science of molecular balance: why simplified reporting is compromising public health.
Research and writing by the ‘HoyLunes’ editorial team, in special collaboration with Dr. Silvia Sánchez-Ramón, Head of the Department of Clinical Immunology, Hospital Clínico San Carlos / UCM.
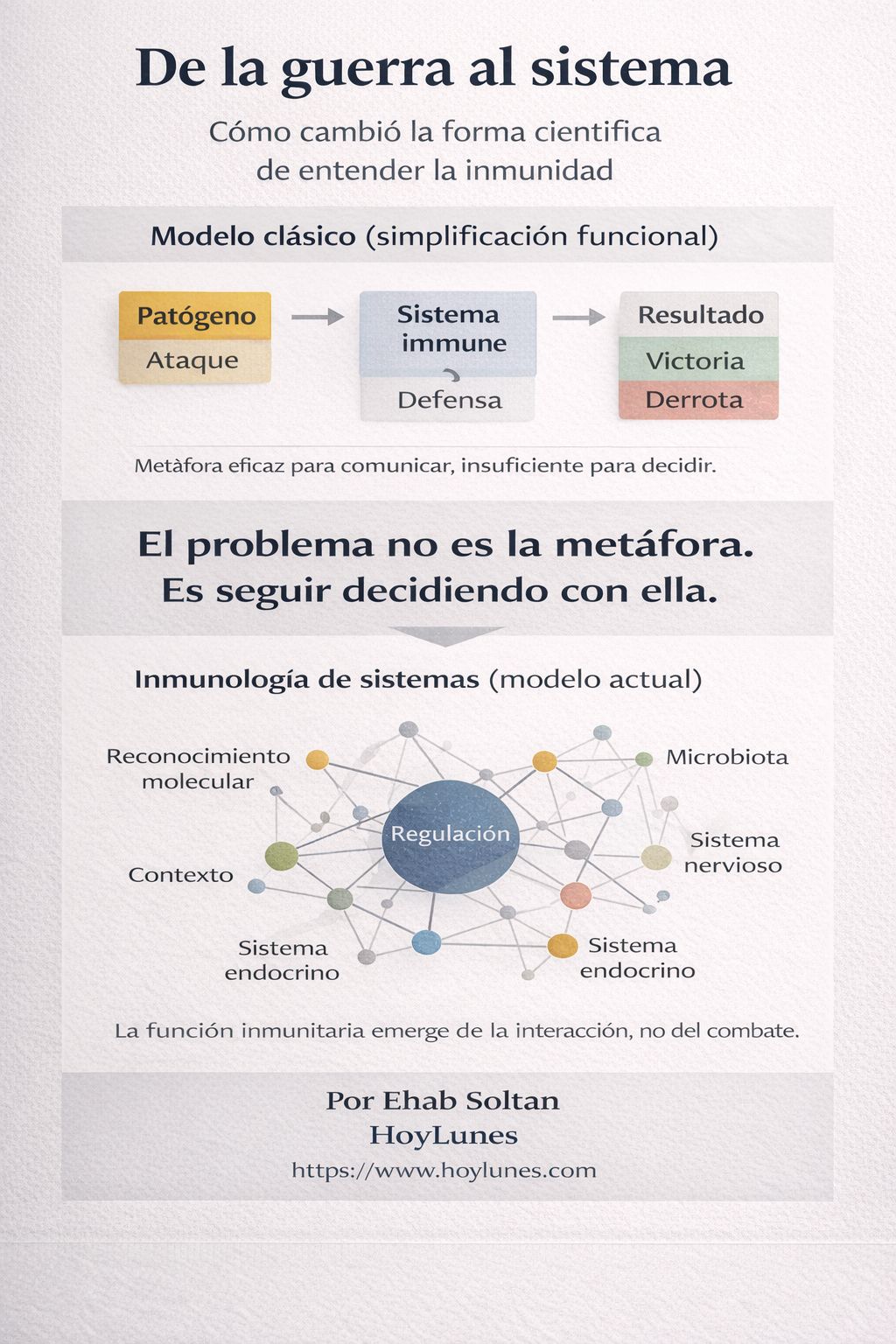
HoyLunes — For decades, medicine has explained the immune system as if it were a battlefield: cellular armies, external invaders, attacks, and defenses that rise or fall. This metaphor was not innocent; it simplified, organized, and allowed for the rapid communication of complex concepts.
Today, however, “that narrative has become a clinical and conceptual burden”.
Persisting in a “trench immunology” is no longer merely a pedagogical imprecision: it is a form of distortion that conditions medical decisions, patient expectations, and public health policies. Contemporary science has demonstrated that the immune system does not operate as a combat force, but rather as “a network of recognition, communication, and regulation”, deeply integrated with other physiological systems.
The uncomfortable question is not whether this metaphor is obsolete—it is—but rather “why we continue to use it” in clinical practice and medical education. For “Dr. Silvia Sánchez-Ramón“, this gap between knowledge and narrative has real consequences: “Current immunology is not understood in terms of victory or defeat, but rather in terms of context, dynamic balance, and adaptive regulation”.
This article does not propose a new, more elegant metaphor. It proposes “abandoning the comfort of binary narratives” and embracing an immunology consistent with the complexity we now recognize.
The Fallacy of the “Self / Non-Self” Binary
The classical view of the immune system as a shock force that rigidly distinguishes between “self” and “non-self” has evolved into a dynamic model. As “Dr. Sánchez-Ramón” aptly describes, the immune system is, in essence, a “molecular recognition system“.
Its primary function includes a constant dialogue with the environment, regulating physiological processes such as development, reproduction, and interaction with the microbiota. Under the doctor’s thesis, the rigid distinction is replaced by an interpretation of danger signals: the system generates ecological relationships and recalibrates its responses according to the state and environment of the organism.
The “Low Defenses” Fallacy
In public debate, immune health is measured on a linear scale. This reductionism has fueled the idea of “stimulating” immunity blindly. However, in “Dr. Sánchez-Ramón’s” clinical experience, the key lies in what is “appropriate to the stimulus and regulated”.
The doctor emphasizes that most relevant immunological pathologies—autoimmune, allergic, or chronic inflammatory diseases—are not due to a “weak” system, but to one that is “dysregulated or excessively reactive”. Ignoring latent genetic predisposition while promoting indiscriminate immune stimulation can be, in many cases, counterproductive.

Immunology as a Distributed Adaptive Network
There is a chasm in the understanding of immunology as an integral system. Immune functions emerge from the dynamic interaction between cells, molecules, and other systems.
“Dr. Sánchez-Ramón” contends that cutting-edge research demonstrates the immune system acts as a “distributed adaptive network“, capable of processing information and regulating homeostasis through bidirectional communication mechanisms with other organs, such as the brain and the endocrine glands. It is at this point that her vision of multiscale communication becomes disruptive to conventional clinical practice, which still tends to view the body in isolated compartments.
A Change in Language is a Change in Responsibility
Transitioning from a “trench immunology” to a “systems immunology” is not a rhetorical exercise. It is an “ethical and professional revision” of how medicine explains itself to itself and to society.
The persistent use of absolute verbs—“strengthen”, “stimulate”, “destroy”—does not merely oversimplify a complex system; it “conveys a false sense of control” that can legitimize poorly contextualized interventions. “Dr. Sánchez-Ramón” is adamant: precision is not an academic luxury; it is a condition for clinical safety.
However, this responsibility does not rest solely with the media. “It also challenges the medical community“, which often reproduces obsolete narrative frameworks out of inertia or communicative convenience.
Accepting that the immune system is a distributed adaptive network forces a rethinking of how we teach and how we decide. Ultimately, it compels us to “think of medicine as a system“.

At ‘HoyLunes’, we understand that this type of reflection finds no place in promotional communication or oversimplified outreach. That is why we operate as a space for external validation, where science is neither defended nor simplified: “it is explained, contextualized, and subjected to critical thinking“.
We thank “Dr. Silvia Sánchez-Ramón” for leading this necessary reflection, which inaugurates our series dedicated to the limits of contemporary medical language. We invite specialists in Immunology, Neurology, Endocrinology, and Internal Medicine to participate in this uncomfortable but necessary dialogue.
Scientific Context of Reference:
Polly Matzinger and the ‘Danger Model’: [[https://www.annualreviews.org/doi/10.1146/annurev.immunol.12.1.991]
Immunology as a complex adaptive system (Nature Reviews Immunology): [[https://www.nature.com/articles/s41577-019-0124-7]
#LenguajeMédico #InmunologíaDeSistemas #PensamientoClínico #SilviaSánchez-Ramón #HoyLunes
‘HoyLunes’ after this espacio a medicos that want to explore the conceptual limitations of their special education, more all of the academic traditional format.